Manage your referral (MYR)
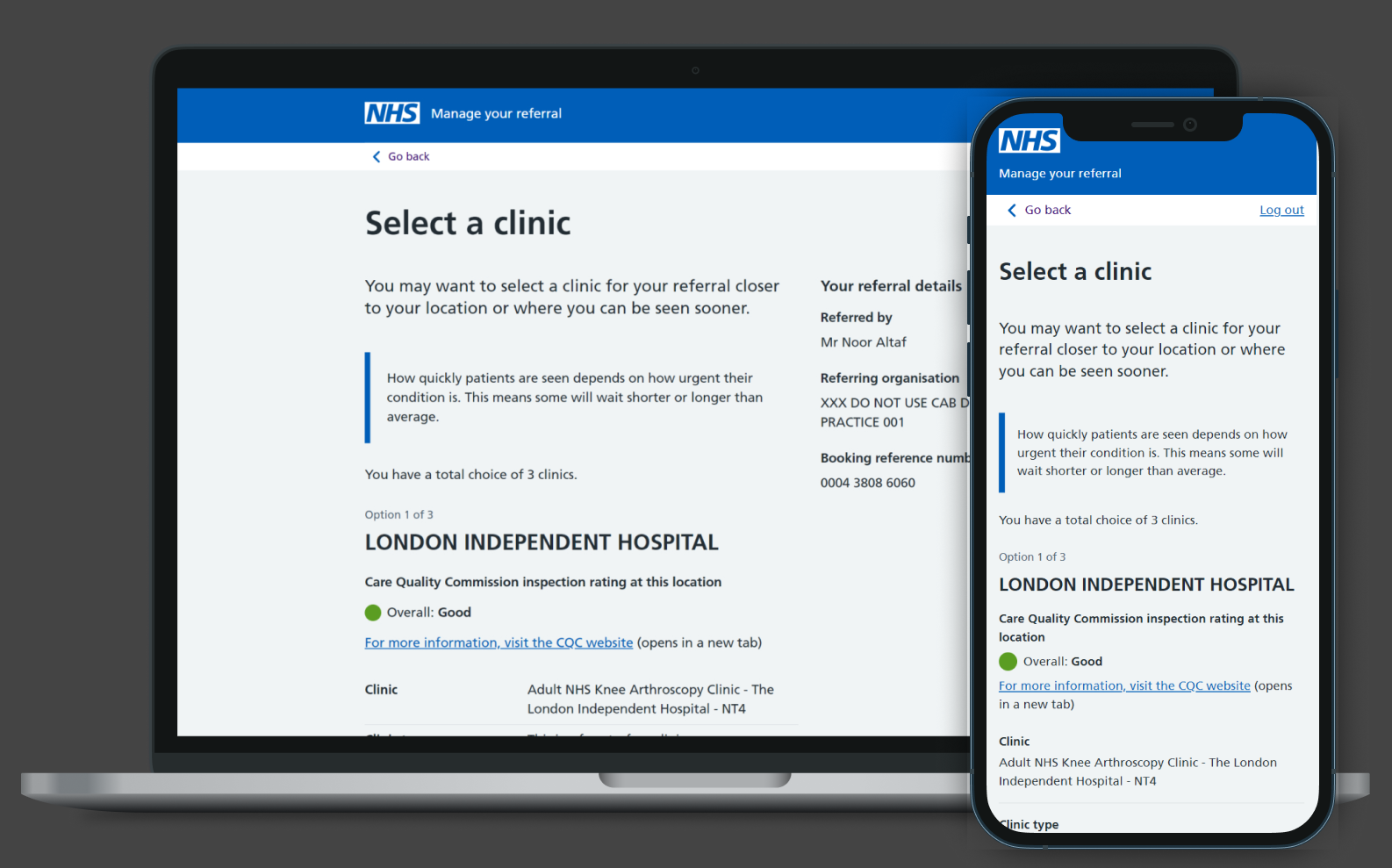
The MYR system is the patient-facing component of e-RS. When clinicians create a shortlist of clinics in e-RS, MYR allows patients to select and manage their referral and any related appointments throughout their NHS care journey. Its functionality includes checking referral status, managing support services, and booking, reviewing, rebooking, or cancelling appointments.
https://refer.nhs.uk/login
Challenge
To identify the primary pain points for MYR users, the research team—working with a Service Designer—analysed patient feedback gathered by GPs, helpdesk operators, and administrative staff. This investigation highlighted several issues: confusing or alarming messaging, insufficient explanation of key statuses (such as cancelled appointments), and a lack of clarity around certain clinic types prior to booking (for example, referral assessment clinics).
These insights proved invaluable in shaping and guiding the subsequent design work.
What we did
Understanding the problem
In order to ascertain the primary pain points of MYR users, the feedback received by GPs, helpdesk operators and administrative staff from patients was closely examined by the research team, who were working in conjunction with a Service Designer. The investigation revealed issues such as confusing and sometimes alarming messaging, insufficient explanation of certain key statuses (cancelled appointments, for example), and a lack of clarity around what certain available clinic types entailed prior to booking (referral assessment clinics, for example).
Gathering these insights was invaluable in providing direction for our onward design work.
Applying the NHSE Design Standard
As noted earlier, the service had been delivered with minimal design input. This led to errors in the use of NHSE design components, poor form validation, limited WCAG 2.0 compliance, weak responsiveness on mobile devices, and a page structure that failed to clearly communicate a patient’s referral status.
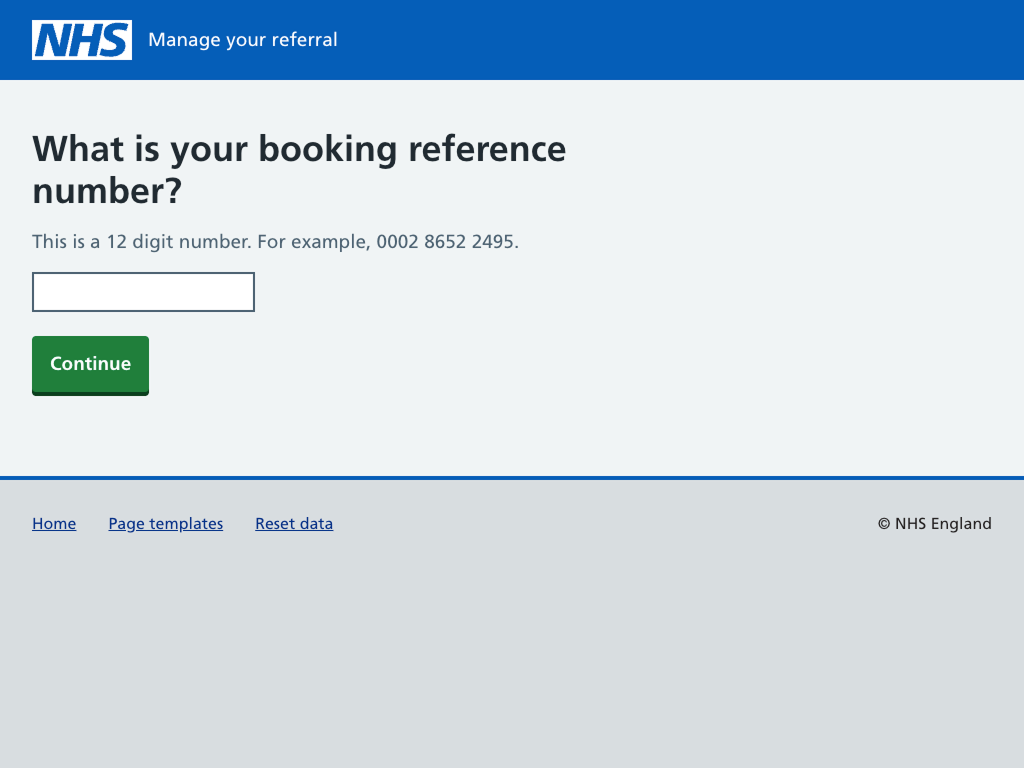
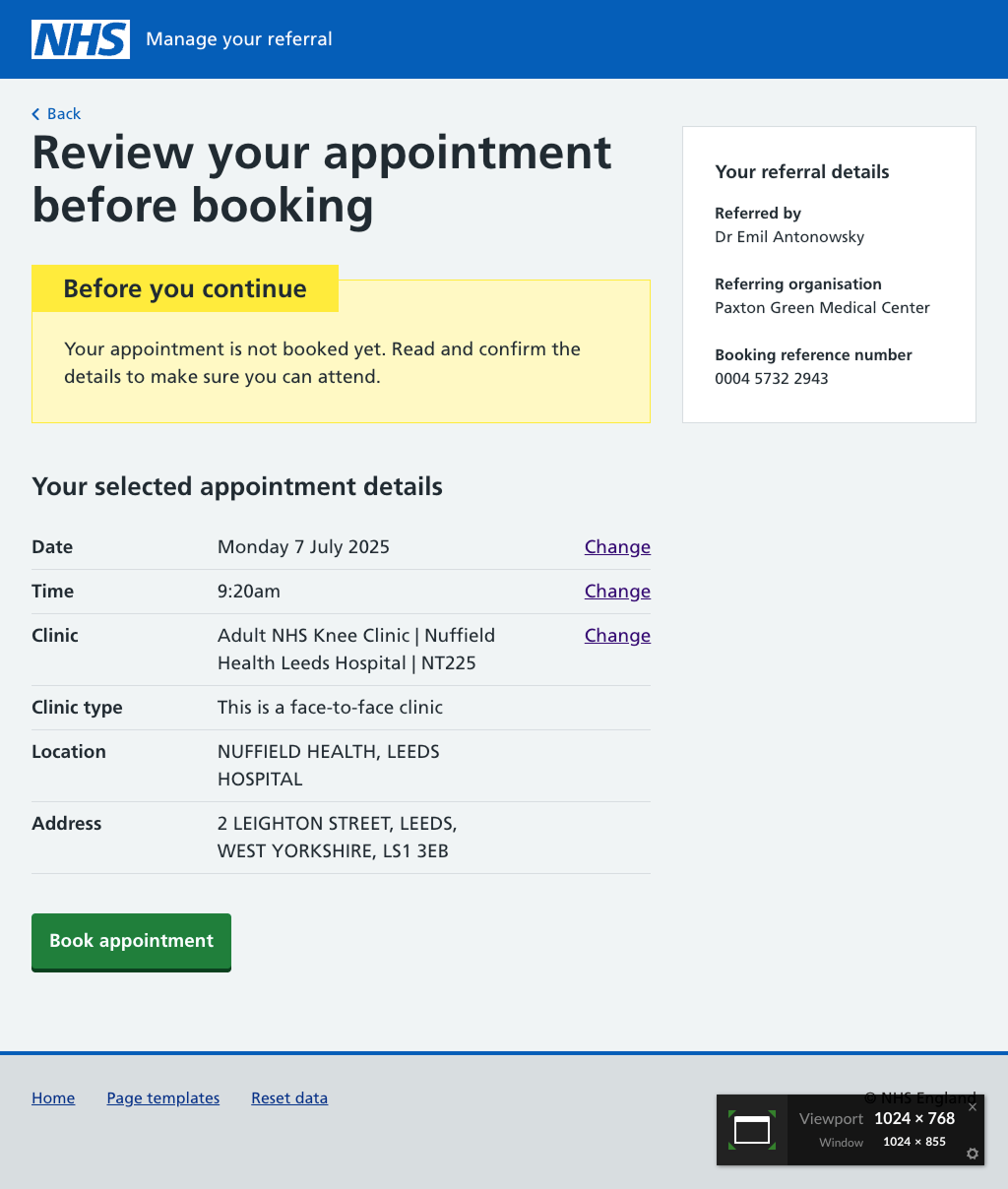
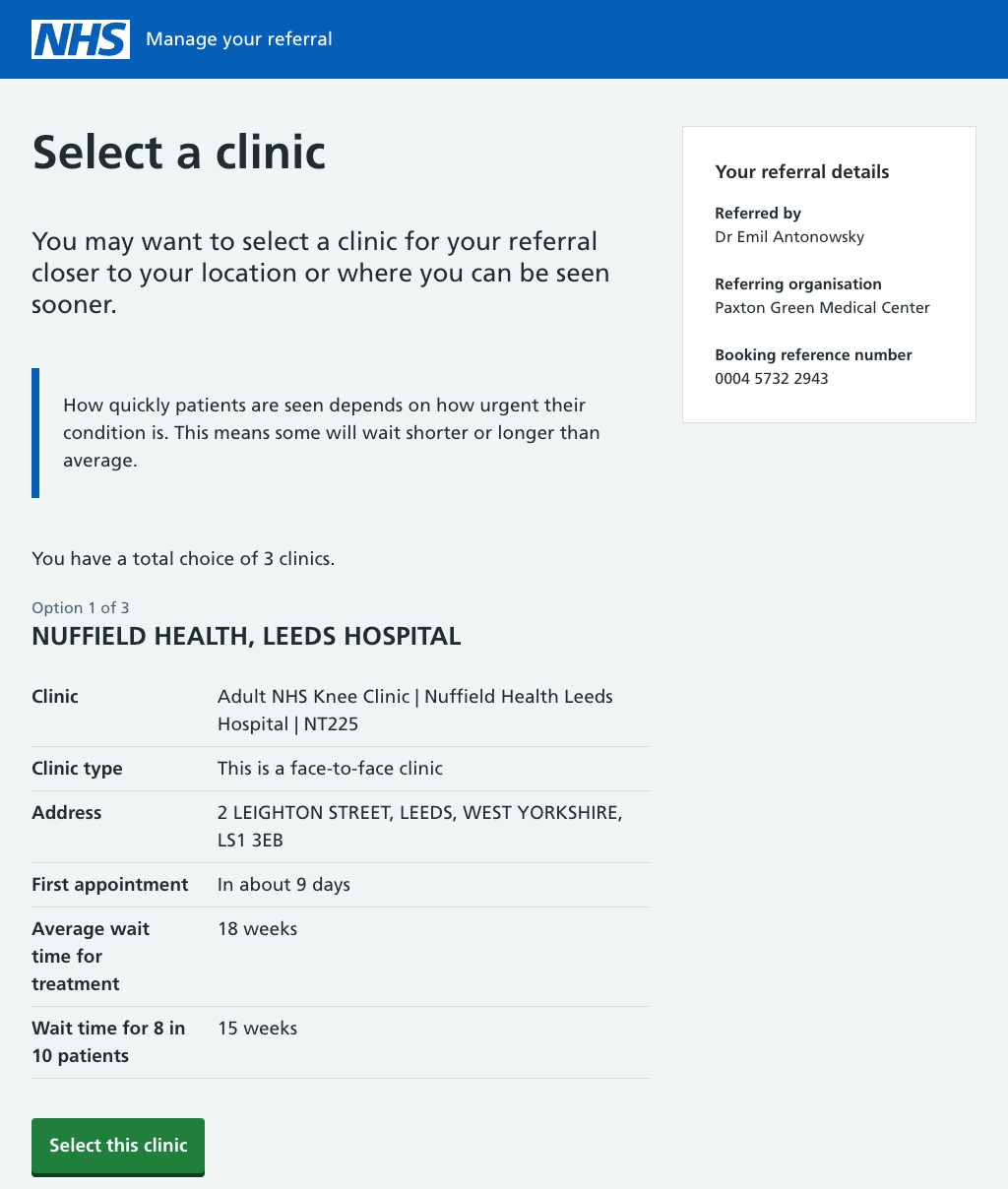
To address this, we introduced a streamlined page design template. Each page now conveys its core purpose clearly through the H1, supported by well-structured sections that guide users through the next steps. We also ensured that the end of every transactional flow (such as booking an appointment) is clearly marked with dedicated Review and Success pages—a feature missing from the legacy service.
Using the NHS Protoyping Kit
Given that this was a patient-facing service, the NHS Prototyping Kit was the natural choice. Its ability to quickly assemble and deploy testable assets compliant with the NHS Design Standard proved invaluable, allowing us to validate assumptions early and identify areas needing refinement.
Building prototypes with the NHS Prototype Kit
Building prototypes with the NHS Prototype Kit
Building prototypes with the NHS Prototype Kit
Content is key
Research showed that on-page messaging was the main source of user distress, making it the natural focus for improvement.
Working with a content designer, subject matter experts, and clinical specialists, we conducted a comprehensive review of the service’s language and tone. The goal was to simplify and clarify on-screen messaging, making it more accessible and less alarming. This helped correct common user misconceptions about the process and significantly reduced anxiety.
Adopting clearer, more accessible language proved pivotal: it improved user experience while preserving the underlying service structure, avoiding costly refactoring. This approach not only saved the client time and resources but also maintained the integrity of service delivery.
Testing with users
Prototypes were constructed and evaluated with users over a period of three months. A side-by-side comparison of the legacy and future service was also conducted with users, with the aim of eliciting meaningful feedback on content and design decisions.
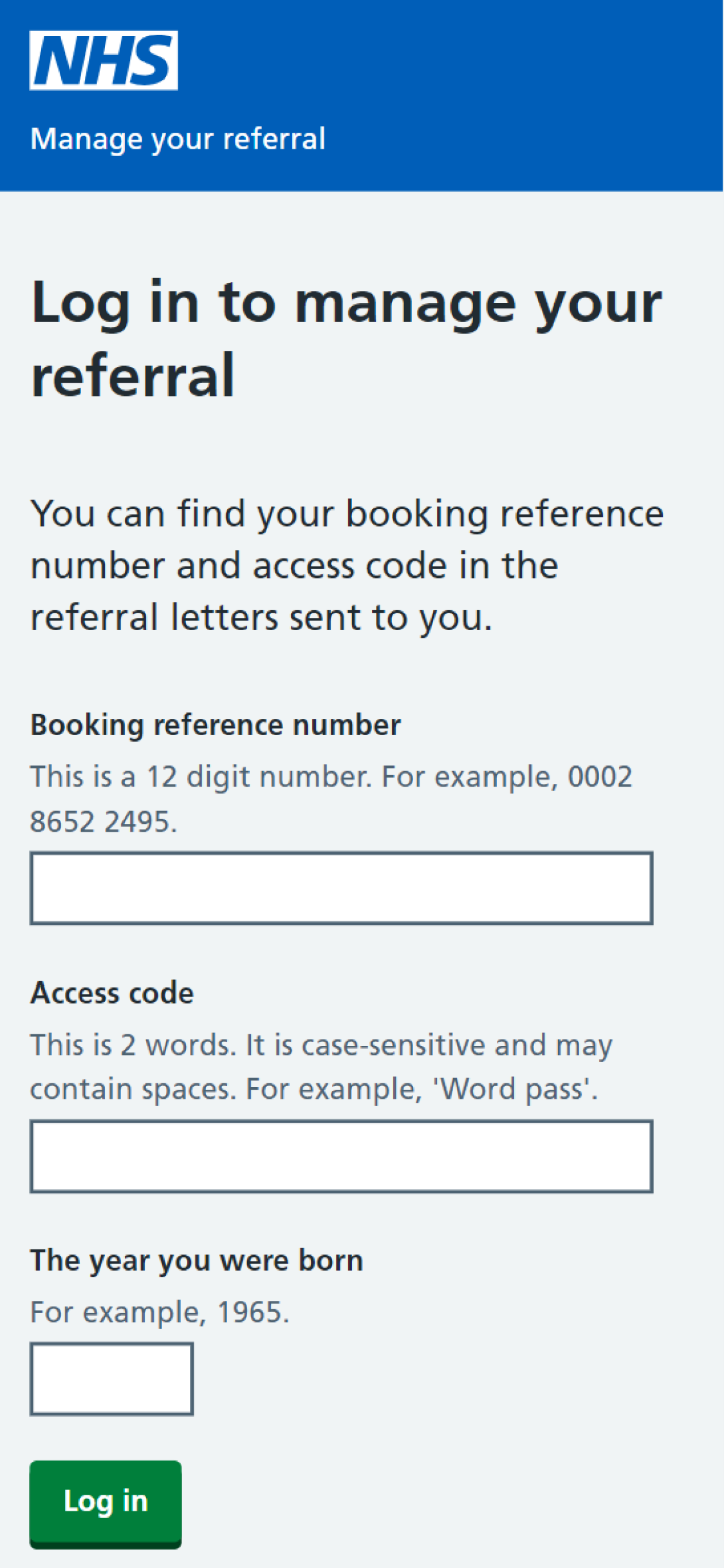
A simple login journey with 2FA ensures patient security and confidentiality
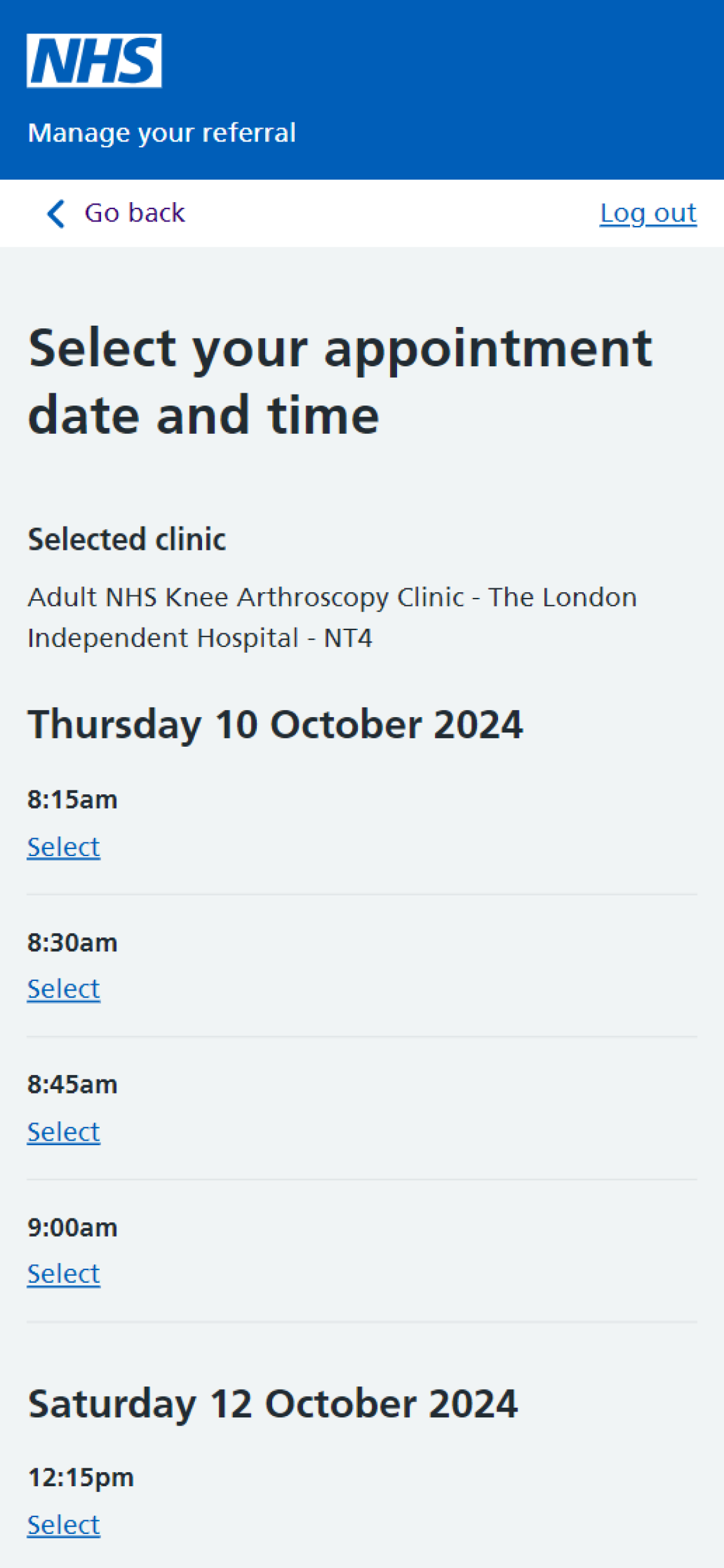
Empowering users to book appointments at a date and time that suits them.
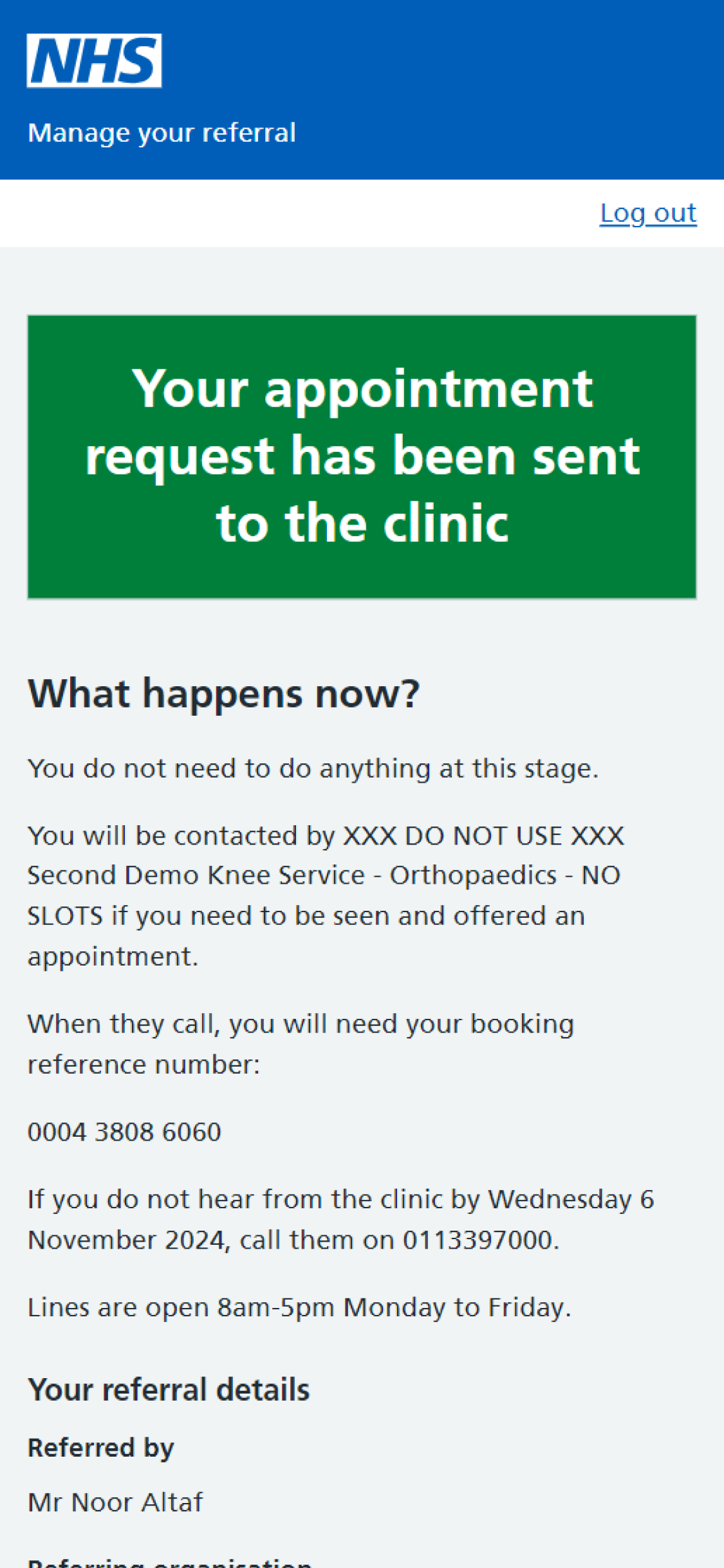
Providing reassurances to the user about what to expect and what they need to do proved to be highly valued by our users.
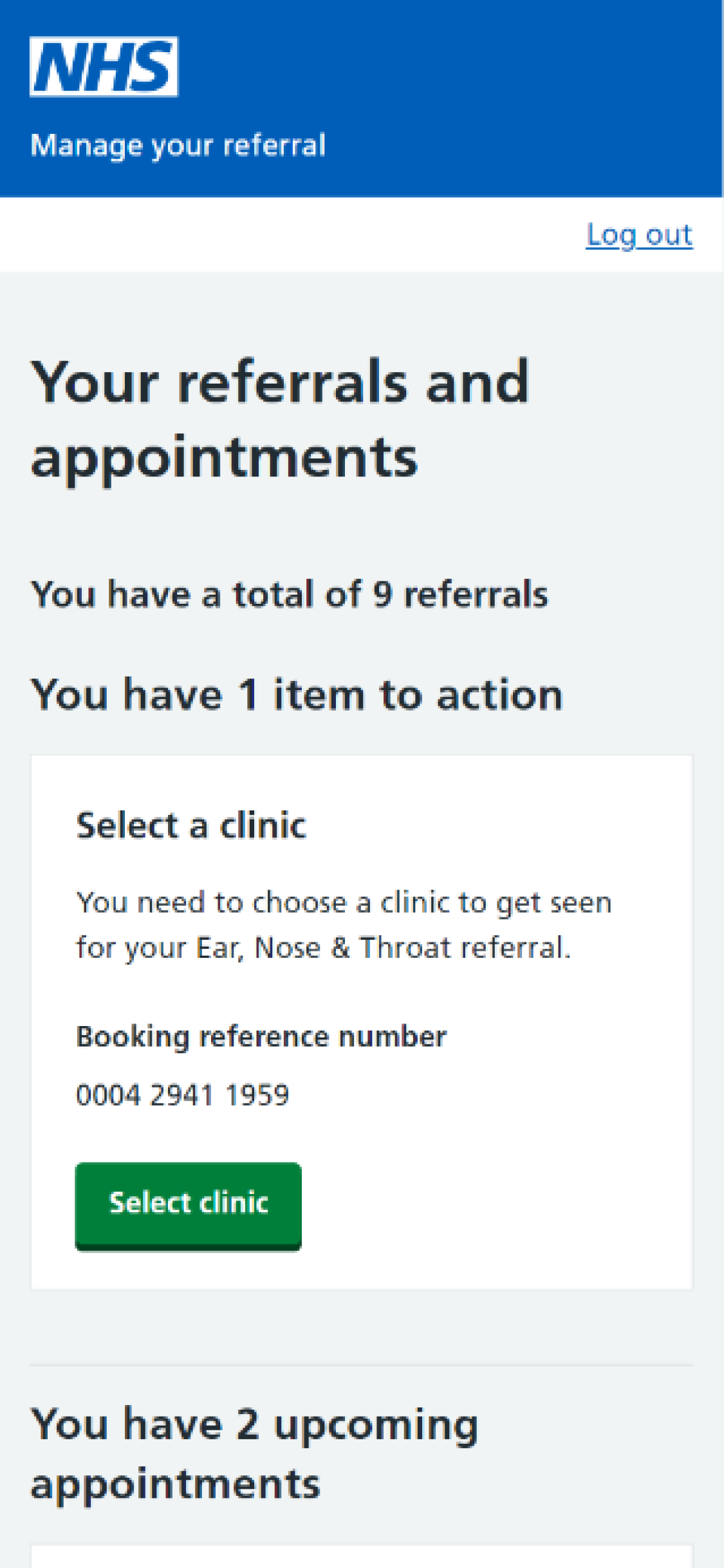
A simple hub page allows users to keep track of all their referrals and appointments.
My role
In my capacity as a consultant for SPARCK/BJSS, I collaborated with both permanent NHSD team members and civil servants. My role was that of Lead Designer. The responsibilities entailed:
Outcomes
Following the implementation of the system, a significant decrease in calls to GP practices and the NHS 111 service has been reported by NHS colleagues. These calls pertained to patients in need of assistance with referrals. The MYR system has been integrated into the NHS app and is also available as a standalone service that can be accessed independently of the NHS app.
